Hairy-cell leukemia (HCL) is a rare and indolent hematologic cancer.1,2 HCL, which is 4 to 5 times more frequent in men than in women, accounts for 2% of all leukemias.3 Approximately 1000 new cases of HCL are diagnosed in the United States annually.3
Patients with HCL can have splenomegaly, varying degrees of leukopenia and/or pancytopenia (resulting in susceptibility to infections), and bone marrow infiltration by atypical cells with prominent cytoplasmic projections (ie, hairy cells).1,2
The decision to treat patients with HCL is based on the presence of symptoms that are secondary to cytopenias and splenomegaly, and the presence of other complications.3 Approximately 10% of all patients with HCL will never require therapy.1
For patients with HCL who are fit and symptomatic, the standard of care is the US Food and Drug Administration (FDA)-approved purine nucleoside analogs cladribine or pentostatin.3 The survival rates of patients with HCL are at least 85% at 5 years of follow-up.2
Despite progress in the management of HCL, this condition is not cured with standard therapy. At relapse, patients with HCL who have poor-risk features (ie, severe anemia, splenomegaly, p53 mutation, unmutated IGHV, IGHV4-34–positive rearrangement, or unmutated BRAF V600E) have disease that is particularly difficult to manage with available treatments.2,4 Substantial opportunities remain for continued research into novel small molecules and biologic drugs for this disease.4
Lumoxiti FDA Approved for Hairy-Cell Leukemia
On September 13, 2018, the FDA approved moxetumomab pasudotox-tdfk (Lumoxiti; AstraZeneca) for the treatment of adults with relapsed or refractory HCL who received at least 2 previous systemic therapies, including treatment with a purine nucleoside analog.5,6
Moxetumomab pasudotox-tdfk is a CD22-directed cytotoxin and is the first of this type of treatment FDA approved for patients with HCL.5,6 The FDA granted the new drug application for moxetumomab pasudotox-tdfk fast track and priority review, and designated it as an orphan drug.5
“Lumoxiti fills an unmet need for patients with hairy cell leukemia whose disease has progressed after trying other FDA-approved therapies,” said Richard Pazdur, MD, Director of the FDA’s Oncology Center of Excellence.5 “This therapy is the result of important research conducted by the National Cancer Institute that led to the development and clinical trials of this new type of treatment for patients with this rare blood disorder,” Dr Pazdur added.
Mechanism of Action
Moxetumomab pasudotox-tdfk is composed of a recombinant, murine immunoglobulin variable domain genetically fused to a truncated form of Pseudomonas exotoxin, which inhibits protein synthesis.6 As a CD22-directed cytotoxin, moxetumomab pasudotox-tdfk binds CD22 on the surface of B-cells and is internalized to bring about ADP-ribosylation of elongation factor 2, inhibition of protein synthesis, and apoptotic cell death.6
Dosing and Administration
The recommended dosage of moxetumomab pasudotox-tdfk is 0.04 mg/kg, administered as a 30-minute intravenous infusion on days 1, 3, and 5 of each 28-day cycle. Treatment with moxetumomab pasudotoxtdfk should continue for a maximum of 6 cycles or until disease progression or unacceptable toxicity.6
Thirty to 90 minutes before each infusion of this agent, patients should be premedicated with an antihistamine (eg, hydroxyzine or diphenhydramine), acetaminophen, and a histamine-2 receptor antagonist (eg, ranitidine, famotidine, or cimetidine).6
Patients should also be hydrated with an isotonic solution (eg, 5% dextrose and 0.45% or 0.9% sodium chloride) for 2 to 4 hours before and after each infusion of moxetumomab pasudotox-tdfk.6
Pivotal Clinical Trial: Study 1053
The approval of moxetumomab pasudotox-tdfk is based on efficacy data from Study 1053, a single-arm, open-label clinical trial of patients with HCL.5,6 Enrolled patients had histologically confirmed HCL or an HCL variant who needed therapy based on the presence of cytopenias or splenomegaly and who had received previous treatment with at least 2 systemic therapies, including a purine nucleoside analog. Eligible patients had serum creatinine levels ≤1.5 mg/dL or creatinine clearance (CrCl) ≥60 mL/min.6,7
Of the 80 patients who participated in this clinical trial, 77 had classic HCL and 3 had an HCL variant.6,7 The patients’ median age was 60 years (range, 34-84 years), and the majority were male (79%), with a baseline Eastern Cooperative Oncology Group performance status of 0 or 1 (98%).6,7 Patients received a median of 3 previous therapies (range, 2-11); all patients received previous purine nucleoside analog therapy, including 29% in combination with rituximab (Rituxan).6
Patients received moxetumomab pasudotox-tdfk as an IV infusion on days 1, 3, and 5 of each 28-day cycle for a maximum of 6 cycles or until documentation of complete response, disease progression, or unacceptable toxicity. The median duration of follow-up was 16.7 months (range, 2-49 months).6,7
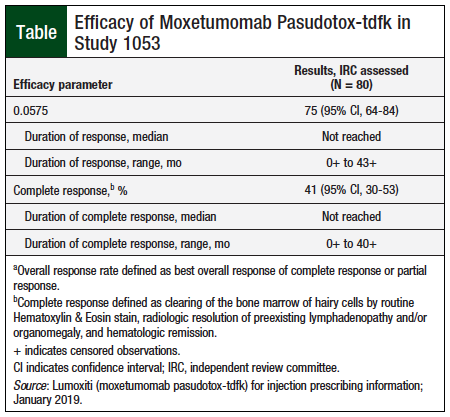
The efficacy of moxetumomab pasudotox-tdfk was based on independent review committee (IRC)-assessed rate of durable complete response, as confirmed by maintenance of hematologic remission (hemoglobin ≥11 g/dL, neutrophils ≥1500/mm3, and platelets ≥100,000/mm3 without transfusions or growth factor for at least 4 weeks) more than 180 days after IRC-assessed complete response. In Study 1053, the durable complete response rate was 30% (95% confidence interval, 20-41).6,7 Additional efficacy outcome measures for moxetumomab pasudotox-tdfk are summarized in the Table.6
Adverse Events
The safety profile of moxetumomab pasudotox-tdfk is based on data from 80 patients with relapsed HCL who received treatment with up to 6 cycles of therapy.6,7 They were exposed to moxetumomab pasudotox-tdfk for a median of 5.7 months (range, 0.9-6.7 months).6
The most common (≥20%) nonlaboratory adverse reactions of any grade were infusion-related reactions (50%), edema (39%), nausea (35%), fatigue (34%), headache (33%), pyrexia (31%), constipation (23%), anemia (21%), and diarrhea (21%).6 The most common (≥5% of patients) severe adverse reactions were hypertension, febrile neutropenia, and hemolytic uremic syndrome (HUS).6
The permanent discontinuation of moxetumomab pasudotox-tdfk because of an adverse event was required in 15% of patients.6 The most common event leading to treatment discontinuation was HUS (5%).6
Moxetumomab pasudotox-tdfk has no contraindications.6
Use in Specific Populations
Moxetumomab pasudotox-tdfk is expected to cause fetal harm. Females of reproductive potential should use effective contraception during treatment and for at least 30 days after the last dose.6
Data are not available to determine if moxetumomab pasudotox-tdfk is present in human milk, or its effects on the breastfed child or on milk production.6
The safety and effectiveness of moxetumomab pasudotox-tdfk have not been established in children.6
Among 129 patients who received moxetumomab pasudotox-tdfk in clinical trials, 31% were aged 65 years or older.6 Exploratory analyses suggest a higher rate of adverse reactions resulting in drug discontinuation in patients aged ≥65 years compared with younger patients (23% vs 7%, respectively) and higher rates of renal toxicity (40% vs 20%, respectively).6 There are insufficient data to identify differences in efficacy of moxetumomab pasudotox-tdfk between younger and older patients.6
Warnings and Precautions
Moxetumomab pasudotox-tdfk prescribing information includes a boxed warning regarding the risks for capillary leak syndrome and HUS, both of which can be life-threatening.6 This drug is also not recommended in patients with severe renal impairment (CrCl ≤29 mL/min).6
Capillary leak syndrome, including fatalities, has been reported with moxetumomab pasudotox-tdfk therapy. Symptoms can include weight gain, peripheral edema, shortness of breath, hypotension, hypoalbuminemia, and hemoconcentration. Patients with capillary leak syndrome should receive appropriate support, including oral or intravenous corticosteroids and hospitalization, as needed.6
Moxetumomab pasudotox-tdfk has been associated with HUS, which is characterized by the triad of microangiopathic hemolytic anemia, thrombocytopenia, and progressive renal failure. The drug should not be used in patients with a history of severe thrombotic microangiopathy or HUS. Intravenous fluids should be given before and after moxetumomab pasudotox-tdfk infusions to prevent this complication. In Study 1053, patients with a platelet count ≥100,000/mm3 also received low-dose aspirin on days 1 to 8 of each 28-day cycle to prevent thrombosis. Patients with HUS should receive appropriate support, including fluid repletion, hemodynamic monitoring, and hospitalization, as needed.6
Because moxetumomab pasudotox-tdfk therapy has been associated with renal toxicity, renal function should be monitored before each infusion and as clinically indicated throughout treatment.6
Infusion-related reactions can occur during any cycle of treatment with moxetumomab pasudotox-tdfk. Before each dose, patients should receive antihistamine and antipyretic premedications. If a severe infusion-related reaction occurs, moxetumomab pasudotox-tdfk should be interrupted for medical management.6
Electrolyte abnormalities, including hypocalcemia, have been observed in patients who received moxetumomab pasudotox-tdfk. These abnormalities can occur together with capillary leak syndrome, HUS, fluid retention, or renal toxicity. Serum electrolytes should be monitored before each dose of moxetumomab pasudotox-tdfk, on day 8 of each cycle, and midcycle.6
Conclusion
Moxetumomab pasudotox-tdfk, the first CD22-directed cytotoxin approved by the FDA, is a new type of treatment for patients with relapsed or refractory HCL, a rare type of leukemia. This novel intravenously administered biologic drug has demonstrated complete and durable responses, with acceptable tolerability, in patients with relapsed or refractory HCL.
References
- National Cancer Institute. Hairy cell leukemia treatment (PDQ)–health professional version. Updated March 23, 2018. www.cancer.gov/types/leukemia/hp/hairy-cell-treatment-pdq. Accessed February 18, 2019.
- Grever MR, Abdel-Wahab O, Andritsos LA, et al. Consensus guidelines for the diagnosis and management of patients with classic hairy cell leukemia. Blood. 2017;129:553-560.
- Troussard X, Cornet E. Hairy cell leukemia 2018: update on diagnosis, risk-stratification, and treatment. Am J Hematol. 2017;92:1382-1390.
- Grever MR, Blachly JS, Andritsos LA. Hairy cell leukemia: update on molecular profiling and therapeutic advances. Blood Rev. 2014;28:197-203.
- US Food and Drug Administration. FDA approves new kind of treatment for hairy cell leukemia. September 13, 2018. www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm620448.htm. Accessed January 31, 2019.
- Lumoxiti (moxetumomab pasudotox-tdfk) for injection, for intravenous use [prescribing information]. Wilmington, DE: AstraZeneca; January 2019.
- Kreitman RJ, Dearden C, Zinzani PL, et al. Moxetumomab pasudotox in relapsed/refractory hairy cell leukemia. Leukemia. 2018;32:1768-1777.